Appendix B provides a comprehensive summary of the results from each of the 13 papers included in this review. These papers explore various aspects related to tics and healthcare, shedding light on important themes and issues.
Unveiling the Challenges in Tics Healthcare
Descriptive Characteristics of Included Papers
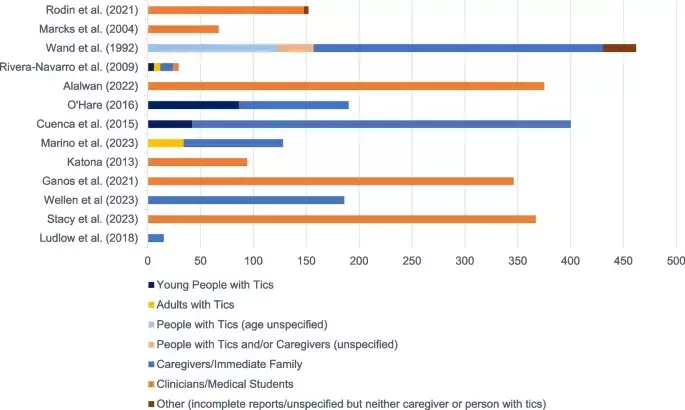
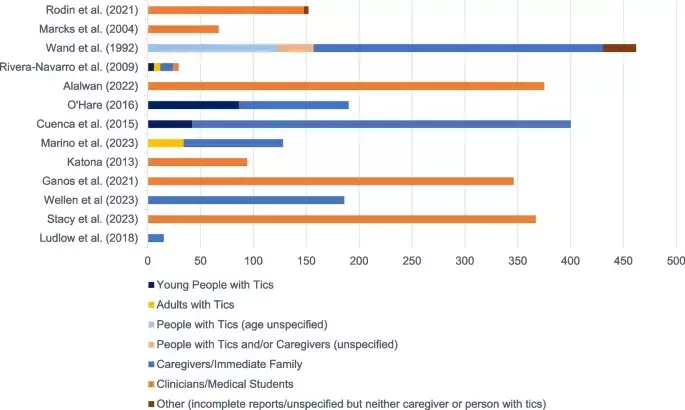
The study selection process is depicted in the PRISMA diagram (Fig. 1). The included studies employed different methodologies - qualitative (n = 2), quantitative (n = 7), or mixed (n = 4). Quantitative and mixed studies used surveys, while qualitative studies used interviews or focus groups. A summary of these studies can be found in Appendix B.All 73 countries represented in the studies have their unique findings. Caregivers formed the largest participant pool (33%), followed by healthcare professionals (HCPs - 32%), medical students (17%), and people with tics (10%). Males dominated among HCPs (60%−80%) and people with tics (65%−85%), while caregivers (52%−93%) and medical students (69%) were mostly female. More details on participant demographics are in Appendix B, along with a distribution graph in Appendix D.The publication dates of the included papers range from 1992 to 2023, with nine papers published in the last 10 years (see Appendix B and D).Summary of Results
Need for Education and Effective ImplementationAll papers emphasized the need for greater professional education in tic disorders across all countries. HCPs interviewed by Rodin et al. [42] highlighted the inadequacy of training on tics.Impact of Limited KnowledgeKnowledge of tics was explored in various aspects. Most HCPs scored between 60 and 80% on tic understanding, lower than for other disorders. Comparisons between care sectors showed no significant difference in HCP knowledge compared to medical students, but knowledge varied among clinical occupations. A significant gap existed between good knowledge scores and low confidence in understanding tics due to limited training opportunities.When young people and caregivers perceived HCPs' sufficient tic knowledge, they felt more confident about their diagnoses. In Uganda, secondary care HCPs were eager to learn more about tics. In Saudi Arabia and the USA, primary and secondary care HCPs wanted to learn about HRT.Secondary care HCPs focused more on treating comorbidities, and MDS members endorsed this. Neurologists and psychiatrists were more likely to manage comorbidities than offer tic-related advice.Limited Support and Unclear Referral ProcessUp to 86% of neurologists offered tic-living advice, but caregivers received limited information. People with tics and caregivers felt unsupported in primary care, leading to dissatisfaction and increased healthcare usage. Primary care HCPs had a limited understanding of treatment options and often prescribed medication. However, 69% of MDS members preferred behavioural interventions as the first-line treatment.Secondary care referrals were necessary due to limited primary care support. Primary care clinicians had limited knowledge of referral sources and often faced rejection.Misinterpretation, Misdiagnosis, and StigmaPrimary and secondary care HCPs underestimated tic prevalence. Tics were often misinterpreted as other disorders. In the UK, GPs were unsure about tic diagnoses. Vocal tics were more likely to be misinterpreted. There were differences in beliefs about tic severity and premotor urges among HCPs.Patients and families felt that HCPs trivialized tic symptoms, and some parents had misconceptions. HCPs also acknowledged tic-related stigma. In Uganda, cultural beliefs affected healthcare seeking. In the UK, parents felt responsible for their child's behavior.Communication between Healthcare Professionals and FamiliesFour studies explored this. Only 45% of secondary care HCPs valued parent input in decisions. 76% of parents preferred collective decision-making. Overuse of clinical language hindered family understanding and relationship development. However, families appreciated GPs who showed compassion and kept them updated.You May Like