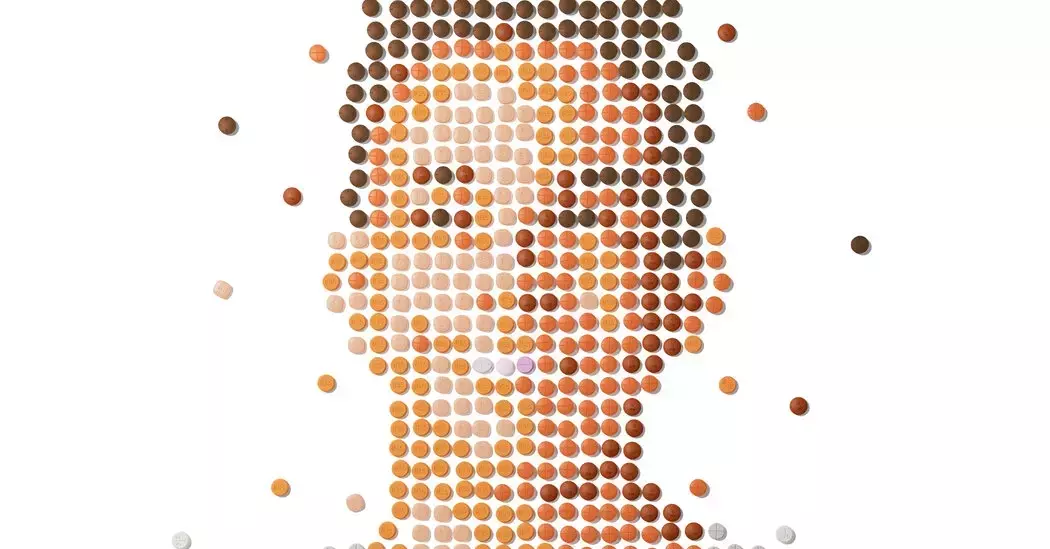
The prevalence of ADHD diagnoses and medication prescriptions has reached unprecedented levels, sparking a reevaluation among scientists about how the condition is defined and managed. According to the Centers for Disease Control and Prevention, over 15% of American adolescents have been diagnosed with ADHD, including a striking 23% of 17-year-old boys, bringing the total number of diagnosed children in the U.S. to seven million. Unlike other medical conditions where diagnosis increases due to breakthrough discoveries, ADHD researchers report a paradoxical situation—our understanding of the disorder has become less clear over time. Recent studies challenge earlier assumptions while simultaneously uncovering new insights into environmental factors influencing symptom progression. This emerging science suggests alternative approaches that could more effectively support millions of young people struggling with focus.
ADHD remains one of the most challenging conditions to diagnose accurately. Symptoms vary widely between individuals, often overlapping with signs of anxiety, depression, childhood trauma, or autism spectrum disorders. Two decades ago, researchers hoped to pinpoint a definitive "biomarker" for ADHD—a singular gene or brain structure difference identifiable through MRI scans. However, these efforts largely proved unsuccessful, leaving diagnosis reliant on subjective assessments rather than objective measures. Compounding this issue, recent research indicates that only approximately one in nine children diagnosed with ADHD exhibit consistent symptoms throughout their childhood. For many others, symptoms fluctuate, sometimes disappearing entirely for years before potentially reappearing. Such findings prompt some experts to reconsider the traditional view of ADHD as an immutable biological trait, proposing instead a model where ADHD represents a transient condition experienced under certain circumstances.
Despite their widespread use, medications like Adderall and Ritalin demonstrate limited long-term efficacy in managing ADHD symptoms. The largest longitudinal study examining ADHD treatments revealed that after 14 months, daily Ritalin doses outperformed non-medication interventions such as therapy or parental coaching. Yet, this advantage gradually diminished, vanishing entirely by the 36-month mark. At that point, children receiving medication showed no greater improvement compared to those undergoing behavioral therapies—or even those who received no intervention at all. These results highlight the need for exploring additional strategies beyond pharmacological solutions to address ADHD effectively.
In light of evolving scientific perspectives, there is growing recognition of the importance of considering environmental influences alongside biological factors when addressing ADHD. By adopting a broader framework that incorporates both aspects, healthcare providers may develop more comprehensive and effective interventions tailored to individual needs. As national concerns about diminishing attention spans persist, embracing innovative approaches offers hope for improving outcomes among the millions of young individuals grappling with focus-related challenges.
