

Michigan's attempt to implement Medicaid work requirements offers a significant lesson for other states now facing similar mandates. Despite a substantial investment of time and resources, and dedicated efforts by state officials to minimize disruption, the program encountered considerable difficulties, underscoring the complexities and potential pitfalls inherent in such policies. The experience reveals how even a well-intentioned implementation can struggle to navigate the intricate web of eligibility, reporting, and exemptions, ultimately putting vulnerable populations at risk of losing crucial healthcare access. This cautionary tale from Michigan serves as a vital point of reference for the many states now grappling with the federal directive to introduce work requirements for Medicaid beneficiaries, prompting a re-evaluation of the human and financial costs involved.
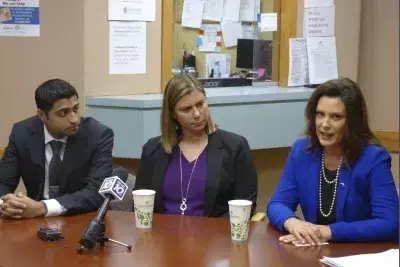
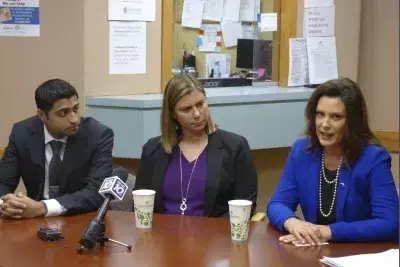
The challenges faced by Michigan in establishing a Medicaid work requirement system highlight the significant administrative burden and the potential for unintended consequences. The state’s previous director of health, Robert Gordon, who oversaw the initial rollout, details how extensive efforts were made to create a system that would prevent large-scale disenrollment. However, the inherent complexities of tracking compliance across a diverse population, managing exemptions, and ensuring effective communication proved immensely difficult. This experience raises serious questions about the feasibility and effectiveness of such mandates on a national scale, especially given the diverse socioeconomic landscapes of different states. The Michigan case study strongly suggests that without careful planning and a deep understanding of potential hurdles, the implementation of work requirements can lead to substantial coverage losses and considerable public health challenges.
The Steep Cost of Policy Implementation
The state of Michigan embarked on a challenging endeavor to implement Medicaid work requirements, a policy inherited from a previous administration. Spearheaded by then-health director Robert Gordon, the effort spanned a year and consumed $30 million in state taxpayer funds. Despite these substantial investments, the system proved unwieldy, struggling to accurately assess and verify the compliance of tens of thousands of Medicaid enrollees. The core objective was to prevent a massive loss of healthcare coverage, yet even with best intentions, the program faced an imminent crisis where a significant number of individuals were poised to lose their health insurance, illustrating the immense operational complexities and financial demands tied to such policy shifts.
In early 2020, Robert Gordon found himself on the verge of disenrolling approximately 80,000 individuals from their Medicaid coverage in Michigan. This predicament arose despite his year-long, $30 million effort to construct a functional system for the state's work requirements. As a former Obama administration official and a Democrat, Gordon was fundamentally opposed to people losing their Affordable Care Act-gained coverage. The work requirements, enacted by a Republican-led state legislature, mandated that Medicaid recipients demonstrate 80 hours of monthly work, volunteering, or job training. Though many enrollees already met these criteria or were exempt, a substantial cohort of 80,000 to 100,000 individuals still faced disenrollment. Gordon noted the catastrophic potential of such numbers, comparing them to the entire population of Flint losing insurance. His team poured resources into building new online and phone reporting systems, aiming to mitigate disenrollment. However, the experience underscored the inherent difficulties of implementing a policy that could lead to widespread coverage loss, regardless of administrative dedication. A federal court ultimately blocked Michigan's policy just before the first COVID-19 cases emerged, sparing those 80,000 individuals from losing vital health coverage during a global pandemic.
Anticipating National Fallout from Work Mandates
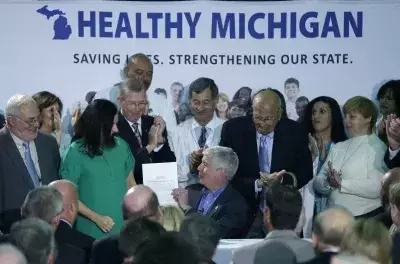
Michigan’s arduous journey with Medicaid work requirements provides a critical blueprint for the 40 states now mandated by federal law to establish similar systems. The Michigan experience underscores the immense financial outlay, administrative complexities, and the profound risk of significant coverage loss that accompany such policies. As the U.S. Congress has recently passed legislation necessitating work mandates for Medicaid, potentially impacting 18 million individuals by 2027, the lessons from Michigan's nearly $30 million, year-long struggle become highly pertinent. Former Director Gordon's cautionary perspective serves as an urgent alert, suggesting that without careful foresight and robust, user-friendly infrastructure, these mandates risk plunging millions into uninsured status, highlighting the delicate balance between policy goals and real-world consequences for healthcare access.
The recent federal legislation signed by President Trump, which extends Medicaid work requirements to 40 states and the District of Columbia, is projected by the Congressional Budget Office to result in 4.8 million more people becoming uninsured by 2034. This significant policy shift requires affected individuals to prove 80 hours of monthly work, volunteering, or job training to maintain their coverage starting in 2027. Republicans advocate for these requirements as a means to address "freeloaders" and manage rising Medicaid costs. However, Democrats argue that such measures undermine a program that has demonstrably saved lives and point to the administrative chaos witnessed in states like Arkansas, where early implementation led to 18,000 individuals losing coverage due to system failures and reporting difficulties. Michigan's experience, while ultimately curtailed by a court ruling, demonstrated the profound challenges even a well-resourced and well-intentioned state faces in preventing inadvertent coverage loss. Robert Gordon warns that despite Michigan’s best efforts—investing in data cross-referencing, re-designing communications, and training staff—hundreds of thousands of people were still at risk. He contends that such policies are not only harmful but also administratively wasteful, diverting critical resources from other public health initiatives, such as addressing high infant mortality rates and the opioid crisis. As other states prepare for these new mandates, Michigan's costly and troubled implementation stands as a stark warning about the potential for widespread disruption and loss of essential healthcare services.
