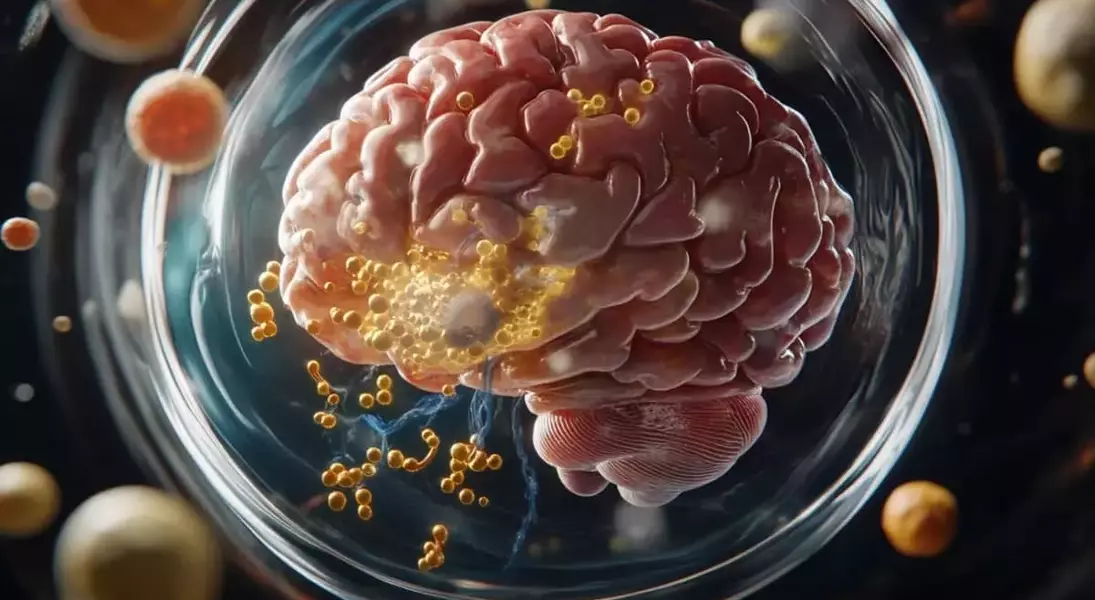
In a remarkable breakthrough, researchers have uncovered the pivotal role of the protein GRAMD1B in managing cholesterol and lipid balance within neurons. This discovery was made possible through the study of "mini-brain" organoids derived from patients with frontotemporal lobar degeneration (FTLD). The findings suggest that altered levels of GRAMD1B can significantly impact cellular processes associated with neurodegeneration, including changes in cholesterol, lipid storage, and tau protein modification. These insights open new avenues for therapeutic interventions targeting GRAMD1B to potentially restore cellular equilibrium and mitigate cognitive decline.
A Novel Pathway in Neurodegeneration
Scientists at The Ohio State University Wexner Medical Center embarked on an innovative journey to explore neurodegenerative mechanisms using human neural organoids, often referred to as "mini-brains." In these models, they identified GRAMD1B as a crucial player in regulating cholesterol and lipid stores within neurons. This protein, previously known for its functions in other parts of the body, has now been linked to neuronal health. By manipulating GRAMD1B levels, researchers observed significant changes in free cholesterol, lipid droplets, and autophagy-related components such as PI3K, phospho-AKT, and p62. Moreover, alterations in GRAMD1B were found to affect phosphorylated tau and CDK5R1 expression, both critical markers of neurodegenerative diseases like FTLD and Alzheimer’s.
The study utilized advanced techniques to examine neurons from both patients and mice, employing sophisticated models that replicate several cell types found in the brain. Through meticulous experimentation, the team demonstrated that blocking GRAMD1B function could reduce free cholesterol and lipid droplets, while knocking down GRAMD1B decreased phosphorylated tau and CDK5R1 expression. These results were published in the prestigious journal Nature Communications, marking a significant leap forward in understanding the complex relationship between lipid dyshomeostasis and tau pathology.
From a broader perspective, this research not only sheds light on the intricate workings of GRAMD1B in the nervous system but also highlights its potential as a therapeutic target for treating FTLD and Alzheimer’s disease.
As noted by Dr. Hongjun “Harry” Fu, the corresponding author of the study, targeting GRAMD1B offers exciting possibilities for developing new treatments that could benefit thousands of Americans affected by these debilitating conditions.
With about 50,000 to 60,000 individuals living with FTLD and an estimated 6.9 million older adults diagnosed with Alzheimer’s dementia, the implications of this discovery are profound. The research was generously supported by various organizations, including the BrightFocus Foundation and the National Institute on Aging.
This groundbreaking work underscores the importance of interdisciplinary collaboration and cutting-edge technology in advancing our understanding of neurodegenerative diseases.
Looking ahead, further studies will be essential to fully harness the therapeutic potential of GRAMD1B modulation.
From a journalist's viewpoint, this discovery serves as a beacon of hope for millions battling neurodegenerative diseases worldwide. It exemplifies how scientific curiosity and rigorous investigation can lead to transformative breakthroughs. As we continue to unravel the mysteries of the brain, such advancements remind us of the immense power of research in shaping the future of medicine. This study not only enhances our comprehension of neurodegenerative processes but also paves the way for innovative treatment strategies that could significantly improve quality of life for countless individuals and their families.
